Background:
Leukemia and the therapeutic treatments for leukemia are both associated with cardiovascular side effects. Heart failure is one of the most identified side effects related to cancer or cancer-related therapies. Evidence suggests a higher risk of HFrEF (heart failure with reduced ejection fraction) and its consequences, there is limited data on the trends of HFpEF admissions in Leukemia patients. In this study, we are using a nationally representative population to study the trends in HFpEF-related admissions and outcomes in elderly Leukemia patients.
Methods:
A retrospective analysis was conducted using the National Inpatient Sample from the 2016-2019 dataset. Elderly patients older than 65 years with leukemia were selected and the trends of HFpEF were studied over these 4 years. In this study, we used both univariable and multivariable regression analysis to adjust the odds ratio and compared and followed the trends over 4 years. Co-primary outcomes were major adverse cardiac and cerebrovascular events [MACCE - all-cause mortality, acute myocardial infarction (AMI), acute ischemic stroke (AIS), and cardiac arrest] in HFpEF patients among the leukemia cohort.
Results:
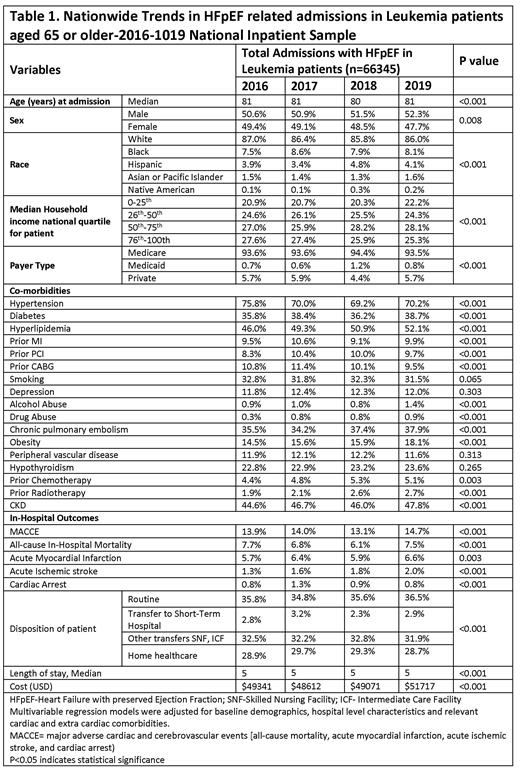
There was a significantly higher prevalence and increasing trends of HFpEF admissions in cohort with leukemia vs non-leukemia between 2016 to 2019 (from 11.6% to 14.4% in leukemia vs. from 10.3% to 13.0%, p trend <0.001). A total of 66,345 admissions with HFpEF in leukemia patients were studied over a period of 4 years, with a median age of 81 [Table 1]. The majority of the patients studied were whites (87%), Medicare patients (93.6%), and urban teaching locations (66.5%). The baseline characteristics trends were matched in all the cohorts and significant comorbidities observed over a period of 2016-2019 were hypertension (75.8% and 70.2%), diabetes (35.8% and 38.7%), hyperlipidemia (46% and 52.1%), prior MI (9.5% and 9.9%), prior PCI (8.3% and 9.7%), prior CABG (10.8% and 9.5%%), alcohol use (0.9% and 1.4%), drug use (0.3% and 0.9%), chronic pulmonary disease (35.5% and 37.9%), obesity (14.5% and 18.1%), prior chemotherapy (4.4.% and 5.1%), prior radiotherapy (1.9% and 2.7%), and CKD (44.6% and 47.8%). On following the trends from 2016 to 2019 we established that Leukemia patients with HFpEF had no significant improvement in in-hospital outcomes of MACCE including all-cause mortality, myocardial Ischemia, acute ischemic stroke, and cardiac arrest between 2016 and 2019 when potential confounders were adjusted. The univariate and multivariable-adjusted odds ratios for all-cause mortality, AMI, cardiac arrest, AIS, and MACCE were 0.97 and 1.04, 1.16 and 1.21, 0.99 and 1.00, 1.49 and 1.49, and 1.06 and 1.12, respectively when compared for Leukemia-HFpEF cohort of 2019 vs. 2016 (p>0.05). Median hospital stay and cost were stable during the study duration without any significantly increasing or decreasing trends.
Conclusion:
There were significantly increasing trends in hospitalizations with HFpEF in elderly leukemia patients without any substantial improvement in acute cardiovascular events between 2016 and 2019. It has been established that cardiovascular outcomes are closely associated with leukemia and related chemotherapy, there is no standardized risk stratification or assessment tool to assess the management of MACEE in Leukemia patients. Furthermore, prospective studies are required to better understand and address the association of leukemia-related treatments and their impact on HFpEF risk and MACCE in the long term.
Disclosures
No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal